|
|
|
The COVID-19 pandemic has wreaked havoc on the fragile economies of the world’s least developed countries (LDCs). The ensuing global recession has led to a slump in external demand for goods and services from LDCs, reduced prices of key exports and constrained inflows of investment and other resources. With limited productive capabilities and diversification, LDCs generally lack the resilience to withstand the multiple economic shocks of the pandemic.
COVID impacts
In 2020, the combined GDP of the 47 LDCs declined by 5%, dropping from pre-pandemic estimates of US$1,057 billion to $1,003 billion.[1] The decline was even higher for LDCs that are the Small Island Developing States (SIDS), i.e. Comoros, Kiribati, Sâo Tomé and Prìncipe, Solomon Islands, Timor-Leste, Tuvalu and Vanuatu. Their combined GDP dropped by approximately 9% compared to pre-pandemic estimates. Most of the 14 LDCs that are members of the Commonwealth experienced similar economic contractions, with the exception of Bangladesh and Tanzania – whose economies grew by around 3% and 2%, respectively. Malawi and Rwanda also experienced marginal growth.
Figure 1: Impact of COVID-19 on GDP of LDCs (2019 vs. 2020)
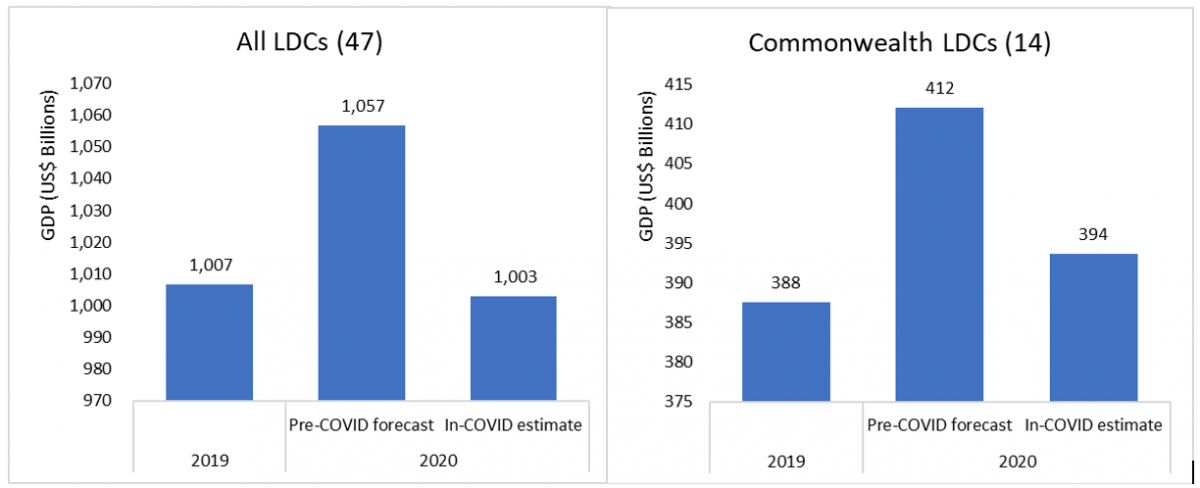
Source: Commonwealth Secretariat using information from the World Bank and IMF
Note: Based on the average growth rates of individual economies using pre-COVID forecasts (October 2019) and in-COVID estimates (January 2021) from the IMF and World Bank. Vanuatu is included as it was an LDC for most of 2020, before its recent graduation.
Aside from the economic losses, the scale of epidemiological-related impact has also been substantial: LDCs have collectively recorded around 1.5 million infections and 28,000 deaths since the onset of the pandemic (see Table 1). The true extent of the health crisis is probably even greater given a significant proportion of infections are likely to go unreported due to limited testing and tracing capabilities.
Vaccine promise?
And while vaccination programmes are underway in some countries, offering a ray of hope, they are yet to begin on any significant scale in LDCs. There is stark inequality in access and distribution, with 75% of all vaccines being administered in just 10 countries, while more than 130 countries have not received a single dose.
Table 1: COVID-19 cases and COVAX vaccine allocations for LDCs
| Region/Group | Population | Cases | Deaths | Allocated doses |
| All LDCs (47) | 1,057,436,185 | 1,600,505 | 28,021 | 74,451,210 |
| Of which | ||||
| Africa and Haiti (32) | 712,149,266 | 585,232 | 11,419 | 47,298,960 |
| Asia (8) | 341,756,433 | 1,010,732 | 16,472 | 26,585,850 |
| Islands (7) | 3,530,486 | 4,541 | 130 | 566,400 |
Note: LDCs are grouped following the UNCTAD classification: https://unctadstat.unctad.org/EN/Classifications.html
Source: Commonwealth Secretariat using information from the WDI and WHO
LDCs do not have the financial resources to negotiate or pre-order vaccines from multiple suppliers, as done by many advanced countries. Their main sources of revenue – typically commodities exports, remittances and tourism income – largely dried up as a result of the pandemic, and financing constraints will remain a major challenge in the short-to-medium term due to the direct and indirect effects of COVID-19.
With a combined population of around one billion, LDCs would need approximately $4 billion to finance two shots of the cheapest Oxford-AstraZeneca vaccine. Given the current limitations in manufacturing capacity globally, and the need to deploy different vaccines to fend off new variants of the virus, the cost of vaccinating entire populations in LDCs could rise exponentially.
Bangladesh is the only LDC with some capacity to manufacture COVID-19 vaccines. Globally, the two leading manufacturers – China and India – are also two of the world’s most populous countries. Given the need of China and India to supply vaccines to their own populations, LDCs that depend on vaccines produced there may experience significant delays to their mass immunisation programmes. Considering this situation, low-income countries, particularly those in Africa – with 33 of the world’s 47 LDCs and 9 of the 14 Commonwealth LDCs – could be left behind.
For most of these countries, the WHO’s COVAX alliance, established to ensure equitable distribution of vaccines, is a silver lining. Through the initiative, an interim allocation of vaccines has been issued for 145 countries, including all LDCs (see Table 2).
Vaccine challenges and the way forward
Even with the vaccines distributed through the COVAX initiative, many LDCs may not complete mass immunisation until 2022 or 2023, or possibly even beyond. Delays in accessing COVID-19 vaccines are likely to lead to sizeable job shedding and the loss of livelihoods (many of which were insecure pre-pandemic), the closure of businesses and a sharp fall in output in the longer-term.
To address these challenges, international institutions and donors need to play a central role in supporting LDCs to attain better access to vaccines. The COVAX initiative offers much promise, but more funding is required if it is to achieve its ambitious goals.[2] Other initiatives, such as the World Bank’s provision of $12 billion in funding for developing countries to finance the purchase and distribution of vaccines, and to fund the development of testing and treatment capacity, can help fill the gap. There is also scope to direct support – through technology transfers, financing and assistance for re-tooling existing facilities – to LDCs such as Bangladesh that have some capacity to manufacture vaccines. The Technology Access Partnership of the UN Technology Bank for LDCs could play an important role.
Coordinated regional approaches can help LDCs to procure and administer COVID-19 vaccines. This requires effective collaboration between governments, international institutions, regulatory partners, donors and the private sector.
LDCs can also look to leverage capacity in the private sector nationally to overcome the distributional challenges associated with implementing vaccination programmes at the scale required to combat COVID-19. For example, collaboration with commercial partners – such as food and beverage companies with cold chain facilities can help governments meet the complex requirements for storing and transporting vaccines.
Table 2: COVID-19 infections, vaccine deployment and COVAX vaccine allocations to LDCs, by country
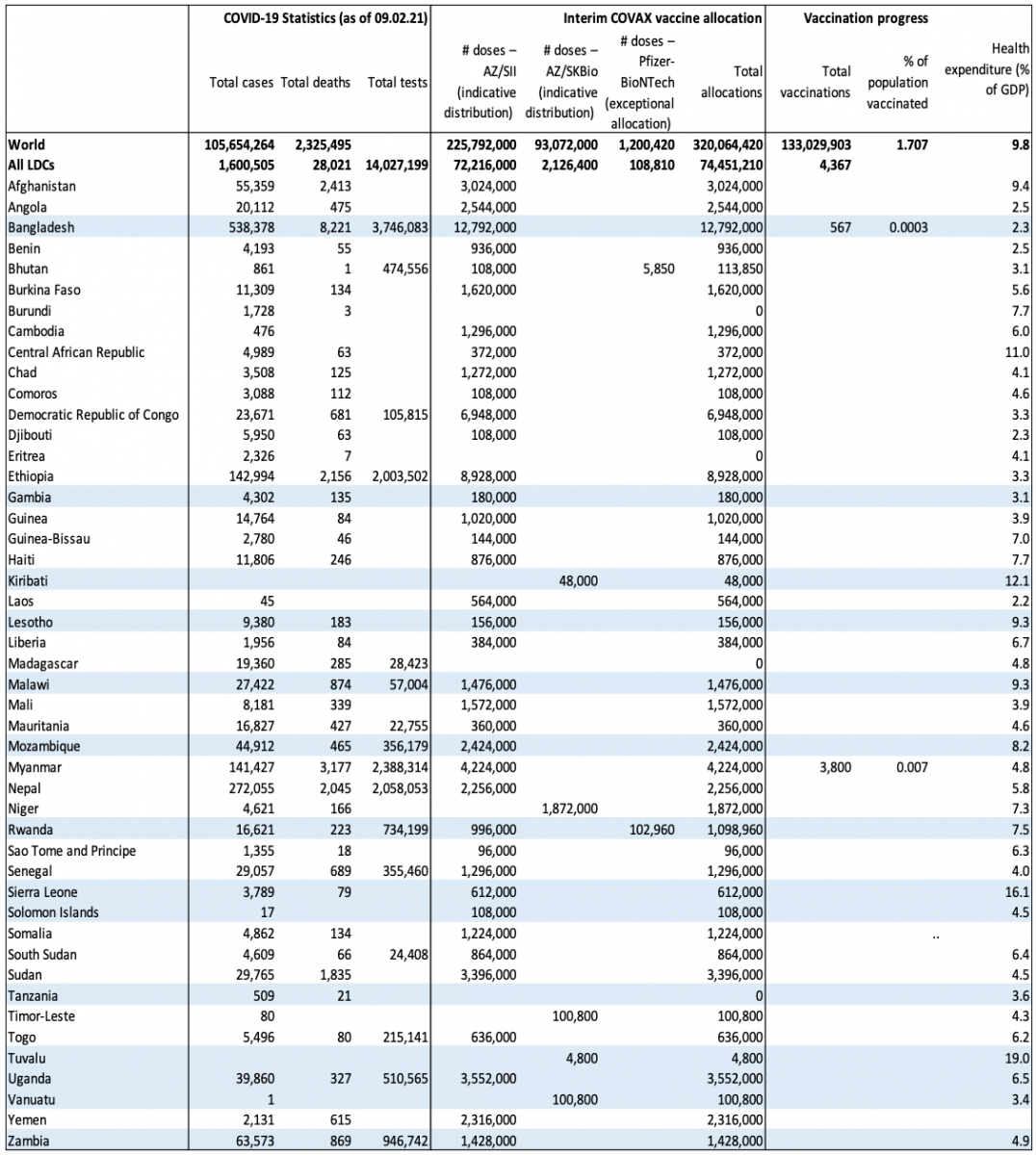 Note: Highlighted LDCs are members of the Commonwealth
Note: Highlighted LDCs are members of the Commonwealth
Source: Commonwealth Secretariat using information from the WDI and WHO
[1] Calculated as the difference between pre-COVID (October 2019) and in-COVID (January 2020) estimates using average growth rates from the IMF and World Bank for individual economies.
[2] According to the WHO, COVAX requires $6.8 billion in funding in 2021 to reach its target of providing access to sufficient doses to inoculate all vulnerable persons across participating countries in the first half of 2021, and reach 20% of their populations by the end of the year.
This piece is part of a dedicated series to spur dialogue, conversations, and debate alongside the WTO's Aid for Trade Stocktaking event taking place from 23 to 25 March. The piece responds to the event's
Theme 4 on GVCs, supply side capacity and the pandemic.
If you would like to reuse any material published here, please let us know by sending an email to EIF Communications: eifcommunications@wto.org.